‘Clients fall off:’ Calgary program helps recently released prisoners with hep C
CALGARY — Imagine adjusting to life after serving prison time, then add mental- health struggles, addiction or homelessness.
Now, throw in hepatitis C, a blood-borne virus that can cause serious liver problems and is several times more prevalent in federal prisons than the general population.
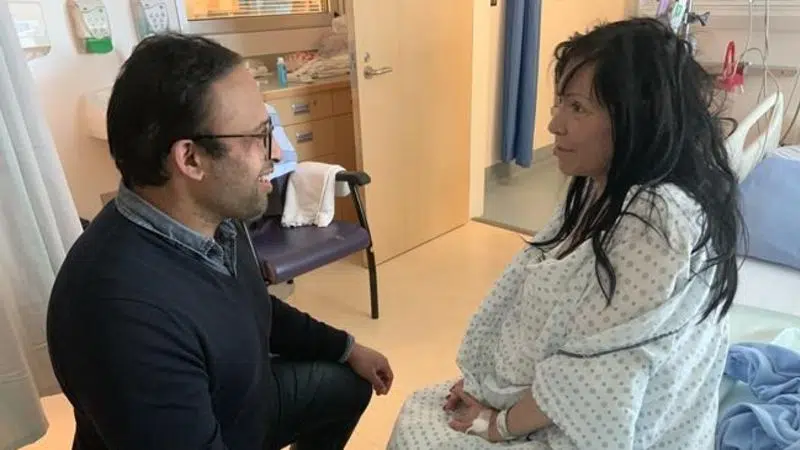
A specialist in addictions and internal medicine who focuses on vulnerable populations has launched a pilot program in Calgary to ensure recently released inmates with a history of injection drug use are screened and treated for the virus.
“It takes a lot of willpower and effort on their end to come out of this. And if we don’t provide them with enough support, they’re not going to be able to,” says Monty Ghosh, a University of Alberta professor who splits his time between Edmonton and Calgary.
